Corneal Collagen Cross-Linking: Advanced Treatment for Keratoconus in Australia

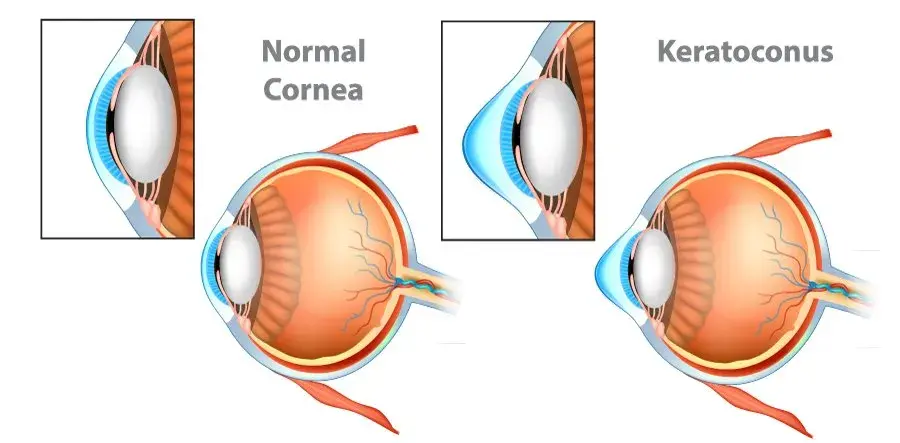
Living with keratoconus can feel overwhelming. The condition causes the cornea to thin and bulge outward, leading to distorted vision and sometimes severe complications if left untreated. But thanks to significant advancements in eye care, particularly in corneal collagen cross-linking, patients now have hope for stronger, healthier corneas and long-term stability.
At Queensland Eye Institute (QEI), patients have access to world-leading cross-linking technology, including customised topography-guided epithelium-on oxygen enhanced cross-linking CXL.
This unique service makes QEI the only clinic in Australia to provide such advanced care for keratoconus. For patients traveling locally and internationally, this treatment represents a breakthrough in modern ophthalmology.
Understanding Keratoconus and Its Impact
Keratoconus is a progressive eye disease where the normally round cornea (the clear outer layer of the eye) becomes thin and develops a cone-like shape. This irregular curvature distorts light as it enters the eye, resulting in blurred or distorted vision.
Patients with keratoconus often notice increasing difficulty with tasks such as reading, driving, or working on digital screens. Early symptoms may be managed with glasses or contact lenses, but as the disease advances, patients may require medical procedures to prevent further deterioration.
If untreated, keratoconus can cause progressive corneal ectasia, severe vision loss, or the need for invasive surgeries such as a corneal transplant. This is where corneal crosslinking treatment plays a critical role.
What Is Corneal Collagen Cross-Linking (CXL)?
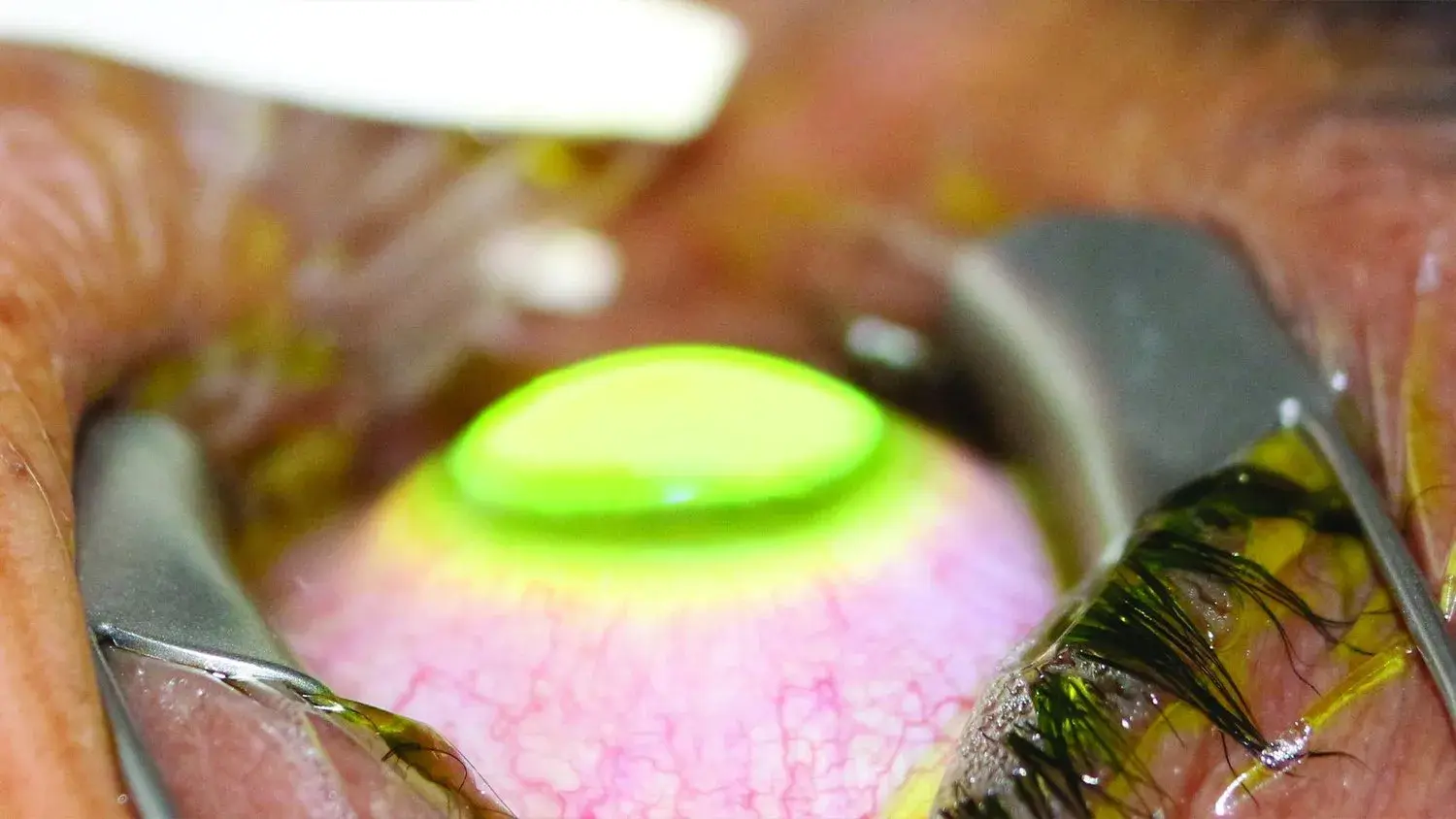
Corneal collagen cross-linking (CXL) is a minimally invasive procedure designed to strengthen a weakened cornea. By applying riboflavin eye drops (vitamin B2) and activating them with ultraviolet light (UV light), the treatment triggers a photochemical reaction that creates new bonds between adjacent collagen molecules in the cornea.
This process increases corneal stiffness, stabilises the corneal shape, and halts the progression of keratoconus. In many cases, it prevents the need for more invasive treatments such as corneal transplantation.
The technique can be applied in two main ways:
- Epithelium-off cross-linking: The corneal epithelium (outer layer) is removed before riboflavin is applied.
- Epithelium-on cross-linking (transepithelial CXL): The outer layer is left intact, reducing discomfort and recovery time.
QEI’s oxygen-enhanced customised topography-guided CXL represents the latest evolution of this procedure, delivering tailored treatment for each patient.

Benefits of Corneal Cross-Linking Treatment
- Stops disease progression: The treatment halts the worsening of keratoconus by strengthening the corneal tissue.
- Outpatient procedure: Patients undergo collagen cross-linking as a same-day treatment under topical anaesthesia.
- Prevents corneal transplant: By stabilising the cornea, many patients avoid invasive surgeries such as corneal transplantation.
- Safe and effective: Clinical studies published in J Cataract Refract Surg confirm its long-term safety and efficacy.
- Improved vision stability: While the main goal is halting progression, some patients notice clearer and more consistent vision.
Recovery Timeline: What Patients Can Expect
After corneal cross-linking procedure, the recovery process varies depending on whether the epithelium was removed. In epithelium-off CXL, patients often experience postoperative pain, light sensitivity, and fluctuating vision for about a week. In contrast, epithelium-on cross-linking generally causes less discomfort and faster surface healing. A bandage contact lens is commonly used to protect the outer layer until it regenerates.
Patients may also be prescribed steroid drops to reduce inflammation and minimise the risk of corneal haze. Over time, the central cornea becomes stronger, and visual stability improves. While some notice early improvements in clarity, the primary goal is halting progression rather than immediate visual gain. Patience is key to successful healing.
How the Corneal Cross-Linking Procedure Works
The corneal cross-linking surgery at QEI is carefully designed to maximise safety and effectiveness. The procedure typically follows these steps:
Preparation:
Patients are given topical anaesthesia (numbing eye drops). The corneal epithelium may be left intact (epithelium-on) or removed (epithelium-off) depending on the treatment plan.
Application of riboflavin:
Riboflavin eye drops are applied to the corneal stroma to saturate the tissue. Riboflavin acts as a photosensitiser, enabling UV light to create collagen bonds.
Ultraviolet light activation:
A focused beam of ultraviolet A light is directed at the cornea. The combination of riboflavin and UV light generates reactive oxygen species, strengthening the collagen fibrils.
Formation of new bonds:
These new bonds between collagen fibers reinforce the corneal tissue, making the cornea stronger and more stable.
Post-procedure care:
A bandage contact lens is often placed on the eye to protect the surface and aid healing.
The entire procedure usually lasts less than an hour and is completed as an outpatient procedure.
Long-Term Results of Cross-Linking Treatment
The long-term outcomes of crosslinking treatment are very encouraging. Clinical research shows that most patients with keratoconus experience halted or slowed disease progression after undergoing collagen cross-linking. Many patients maintain stable vision for years, reducing the risk of needing a corneal transplant.
In some cases, the corneal shape improves slightly, which can lead to better vision with glasses or contact lenses. The strengthened collagen fibrils help maintain a stable and healthy cornea, lowering the risk of complications such as severe corneal scarring or stromal haze.
With proper monitoring and follow-up, cross-linking provides patients with long-lasting reassurance that their vision is preserved and that they can continue everyday activities with confidence.

Recovery and Healing After Cross-Linking Treatment
Healing after corneal cross-linking procedure depends on whether the epithelium was removed. Patients often experience postoperative pain or discomfort for about a week, especially after epithelium-off CXL.
During recovery, patients may experience:
- Temporary corneal haze or stromal haze.
- Corneal swelling or irritation.
- Light sensitivity, tearing, or mild redness.
Doctors usually prescribe steroid drops and lubricating eye drops to aid healing and reduce inflammation. A bandage contact lens may remain in place until the outer layer (epithelium) heals completely.
Most patients notice gradual improvement in comfort within days to weeks, though vision stabilisation may take several months.
The Role of Riboflavin in Cross-Linking
A critical component of corneal cross-linking treatment is the use of riboflavin vitamin B2 eye drops. Riboflavin penetrates the corneal stroma and, when activated by ultraviolet A light, produces reactive oxygen species that strengthen the collagen bonds. This process creates new bonds between collagen fibers and significantly increases corneal stiffness.
In simple terms, riboflavin acts like a catalyst, ensuring that the cornea absorbs the UV energy safely and effectively. Without riboflavin, the UV exposure would not generate the required photochemical reaction. The result is a cornea stronger and more stable, slowing or halting disease progression in patients with keratoconus and related thinning disorders.
Conditions Treated with Corneal Cross-Linking
Corneal cross-linking is most widely used as a keratoconus treatment, but it is also effective in managing other corneal diseases:
- Patients with progressive keratoconus: The primary candidates for CXL, especially those with thin corneas or early signs of vision deterioration.
- Pellucid marginal degeneration: Another corneal thinning disorder that responds well to crosslinking treatment.
- Terrien marginal degeneration: Rare but can also benefit from stabilisation.
- Post-refractive surgery complications: Conditions such as progressive corneal ectasia after LASIK or radial keratotomy can be treated with CXL.
- Infectious keratitis: Some cases of bacterial or fungal infection may respond to activated riboflavin therapy.
- Herpetic keratitis and microbial keratitis: Careful case selection can allow CXL to be used to control infection and reinforce the cornea.
Potential Risks and Complications
Like any medical procedure, corneal cross-linking surgery carries potential risks. While rare, patients should be aware of possible complications:
- Corneal haze or stromal haze that may persist.
- Severe corneal scarring in advanced cases.
- Risk of sterile infiltrates or, rarely, infectious keratitis.
- Temporary vision fluctuations during recovery.
- Rare progression of disease despite treatment.
These risks are minimised at advanced centres such as QEI, where world-leading technology and highly experienced surgeons ensure the safest possible outcomes.
Why Choose QEI for Corneal Collagen Cross-Linking in Australia
Patients seeking corneal collagen cross-linking in Australia deserve access to the highest standard of care. At QEI, Dr Brendan Cronin and the team are proud to be the only clinic in Australia offering customised topography-guided epithelium-on oxygen enhanced crosslinking treatment from Glaukos.
This technology allows:
- Personalised treatment tailored to each cornea’s unique shape.
- Reduced discomfort with epithelium-on techniques.
- Faster healing and less risk of complications.
- Safer treatment for patients with keratoconus, including those with thin corneas.
For patients across Keratoconus Australia and beyond, QEI represents a centre of excellence for advanced care.
Final Thoughts
Corneal collagen crosslinking is more than just a treatment—it’s a life-changing procedure that offers patients the chance to preserve vision, prevent disease progression, and avoid invasive surgeries like corneal transplantation.
By strengthening the corneal tissue through riboflavin vitamin B2 eye drops and UV light, this innovative crosslinking procedure helps make the cornea stronger, healthier, and more resilient against the challenges of keratoconus and related conditions.
At QEI, patients benefit from the very latest innovations in cross-linking CXL, ensuring world-class outcomes in a safe, patient-focused environment. For individuals facing keratoconus, this treatment provides not only stability but also hope for a brighter, clearer future.
