Recurrent Corneal Erosion Treatment

Recurrent corneal erosions (also known as recurrent erosion syndrome) can be a painful and frustrating condition, characterized by repeated episodes of the cornea’s surface cells (corneal epithelial cells) detaching from the underlying tissue. Fortunately, advancements in treatment options have significantly improved outcomes for individuals experiencing this condition.
Introduction to Treatment of Recurrent Corneal Erosion
Recurrent corneal erosion syndrome (RCES) is a common and often distressing eye condition marked by repeated episodes where the corneal epithelium—the thin, protective outer layer of the eye—breaks down. This breakdown can result in severe pain, blurred vision, and significant discomfort, primarily upon waking. The corneal epithelium is crucial for maintaining clear vision and serves as a protective barrier against environmental irritants and infections.
When this layer is compromised, as in recurrent corneal erosion, patients may experience ongoing symptoms that disrupt daily life. RCES can arise from a variety of causes, including previous eye injuries, underlying corneal dystrophies, or chronic dry eye syndrome. Understanding the underlying factors that contribute to recurrent corneal erosion is crucial for effective management and long-term relief.

Causes and Risk Factors
The development of recurrent corneal erosion syndrome can be traced to both traumatic and non-traumatic origins. Traumatic causes often involve direct injury to the corneal surface, such as a scratch from a fingernail or contact with plant material, which can disrupt the epithelial basement membrane and impair the routine healing of the corneal epithelium. Non-traumatic causes are frequently linked to underlying conditions like epithelial basement membrane dystrophy (EBMD), a common corneal disorder that weakens the attachment between the epithelium and the underlying tissue, making recurrent corneal erosions more likely.
Additional risk factors include chronic dry eye, ocular rosacea, and meibomian gland dysfunction, all of which can compromise the health of the corneal surface. Individuals who have undergone eye surgeries, such as cataract surgery or refractive surgery, may also be at increased risk due to changes in the basement membrane and corneal healing response.
Symptoms and Diagnosis
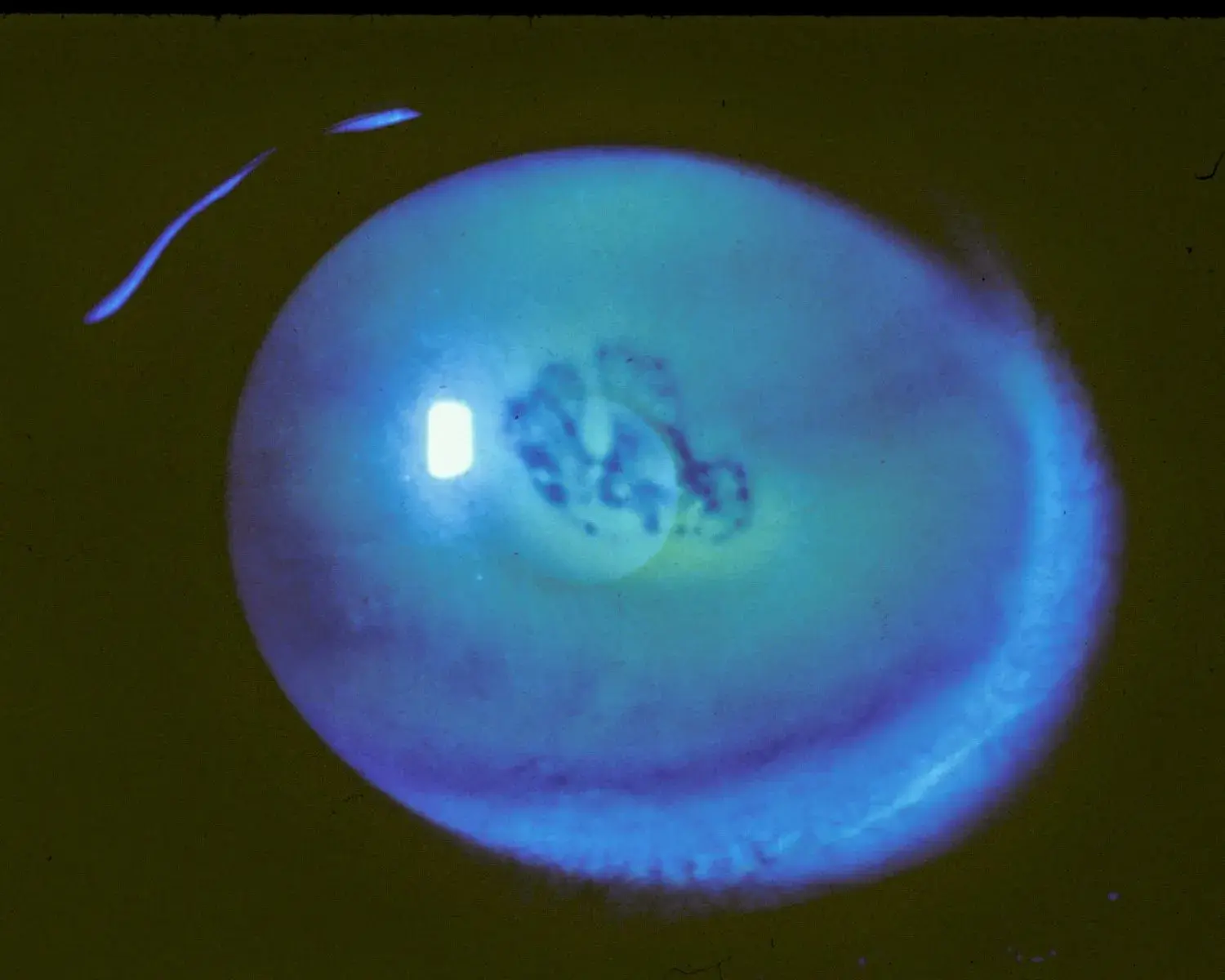
Recurrent corneal erosion syndrome typically presents with sudden episodes of severe pain, often occurring upon awakening when the eyelids first open. Other common symptoms include persistent irritation, redness, excessive tearing, and light sensitivity. Blurred vision and discomfort can significantly impact daily activities. Diagnosis of recurrent corneal erosion relies on a comprehensive eye examination, where an ophthalmologist will assess the corneal epithelium using slit-lamp biomicroscopy and fluorescein staining to highlight any epithelial defects.
In some cases, advanced imaging techniques like in vivo confocal microscopy are used to provide a detailed view of the affected eye and confirm the diagnosis. A thorough medical history and careful examination are crucial for distinguishing RCES from other causes of ocular discomfort and for guiding appropriate treatment.

1. Lubricating Eye Drops and Ointments
The first line therapy for recurrent corneal erosions often involves lubricating eye drops and ointments. Hypertonic saline solution or ointment can also be used as an adjunctive or alternative conservative treatment; by creating an osmotic gradient, hypertonic saline draws excess fluid from the corneal epithelium, promoting epithelial adhesion and healing.
These provide temporary relief by increasing the moisture on the cornea’s surface and reducing friction during blinking. Regular and consistent use of lubricating agents can help prevent further erosions and promote healing of existing ones, especially in patients with corneal recurrent erosion syndrome or underlying epithelial basement membrane abnormalities.
2. Bandage Contact Lenses
Bandage contact lenses (a type of therapeutic contact lens) are another effective treatment option. These soft, therapeutic lenses protect the cornea, promote healing, and reduce pain by creating a barrier between the eyelid and the damaged surface.
They also help maintain a more stable tear film, which facilitates the healing process. Bandage contact lenses are typically worn for a few days or weeks, allowing the cornea to recover and reduce the risk of recurrent corneal erosions related to mechanical trauma or corneal abrasion.

3. Steroid Eye Drops
Steroid eye drops (also known as topical corticosteroids) can help recurrent corneal erosions by reducing inflammation and promoting the healing process of the cornea’s surface. In some treatment regimens, steroid eye drops may be used in conjunction with oral tetracycline or oral doxycycline as part of a prophylactic treatment regimen to enhance treatment outcomes.
4. Doxycycline Tablets
Oral doxycycline is one of several medical treatments used for recurrent corneal erosions. Although primarily known for its antibacterial properties, doxycycline’s benefits for corneal health extend beyond its antimicrobial action. One key mechanism of doxycycline’s effectiveness in recurrent corneal erosions is its ability to inhibit matrix metalloproteinases (MMPs), enzymes that degrade the extracellular matrix of the cornea. By suppressing MMP activity, doxycycline helps maintain the integrity and stability of the corneal epithelial basement membrane and basal epithelial cells, reducing the risk of erosions.
Additionally, doxycycline possesses anti-inflammatory properties. It can modulate the immune response, reducing inflammation in the cornea and promoting the healing process. This anti-inflammatory effect contributes to the alleviation of symptoms and the prevention of further erosions, particularly in cases associated with diabetes mellitus or anterior basement membrane dystrophy.

5. Debridement and Epithelial Membrane Removal
In cases where the corneal epithelium does not adhere properly—such as when there is loose epithelium or a loose epithelial layer—gentle debridement or removal of the loose membrane may be necessary. This procedure enables the regrowth of a new, healthy layer of epithelial cells, thereby reducing the risk of future erosions.
Following debridement, protective measures such as bandage contact lenses or therapeutic contact lenses are often employed to aid in the healing process. Debridement is particularly beneficial in cases of map dot fingerprint dystrophy, epithelial microcysts, or bowman layer disorders where the underlying structure is compromised.
6. Surgical Treatments
For recalcitrant recurrent corneal erosions resistant to conservative treatments, surgical treatment options may be considered. These may include procedures like excimer laser phototherapeutic keratectomy (PTK), which is performed using an excimer laser, or epithelial debridement with diamond burr polishing. Superficial keratectomy and anterior stromal micropuncture are other surgical options for severe or refractory cases.
These minimally invasive surgical procedures aim to create a smooth anterior portion of the cornea and improve epithelial adherence. Before these interventions, topical anesthesia is typically administered to ensure patient comfort. The goal of these surgical techniques is to promote stronger adhesion, facilitate epithelial healing, and reduce the occurrence of erosions.
Some procedures specifically target the underlying stroma and anterior stroma to promote better adhesion of basal epithelial cells. Maintaining an intact epithelium during specific procedures can facilitate faster recovery and reduce complications.
However, corneal haze can be a potential complication following procedures such as PTK or diamond burr polishing. Persistent epithelial defects may require advanced management, including surgical options.
Adjunctive therapies, such as cryopreserved amniotic membrane, autologous serum eye drops, or other treatments, can be considered for recalcitrant cases to promote adhesion and enhance healing.
Complications of Corneal Erosion
If recurrent corneal erosion syndrome is not managed correctly, it can lead to several serious complications. Persistent or untreated erosions may lead to corneal scarring, which can cause permanent vision impairment and decrease overall visual acuity.
The compromised corneal surface also increases the risk of bacterial infection and infectious keratitis, a potentially sight-threatening condition that can cause severe pain and further damage to the eye. Chronic cases of RCES may contribute to the development of other ocular surface diseases, such as dry eye syndrome and ocular rosacea, further complicating management.
In some patients, recurrent corneal erosions may present as sudden-onset symptoms or an acute attack, particularly in those with anterior basement membrane dystrophy or corneal epithelial basement membrane irregularities. Early recognition and prompt treatment of recurrent corneal erosion are crucial to prevent complications and maintain long-term eye health.
Recurrent Erosion Prevention
Preventing recurrent corneal erosion involves a proactive and comprehensive approach that targets both the underlying causes and contributing risk factors. Medical treatment options, such as topical antibiotics, topical steroids, and topical corticosteroids, can help control inflammation and prevent infection. Additionally, preservative-free artificial tears are essential for maintaining a healthy, lubricated ocular surface.
For patients with persistent or severe RCES, surgical interventions like anterior stromal puncture, phototherapeutic keratectomy, or other minimally invasive laser treatment methods may be recommended to promote stronger epithelial adhesion and reduce the likelihood of future erosions. Additionally, prophylactic treatment and structured treatment regimens can play a crucial role in maintaining long-term stability.
To reduce risk, patients should avoid mechanical trauma to the cornea, wear protective eyewear during activities that pose a risk of injury, and maintain good eye hygiene. Regular follow-up with an eye care professional is crucial to monitor the condition, assess treatment outcomes, and adjust therapy as needed.
In some cases, prospective randomised trials have highlighted that consistent management strategies significantly reduce recurrence rates.
Conclusion
The treatment of recurrent corneal erosions requires a multifaceted approach tailored to the individual’s condition. By utilizing various medical treatments, prophylactic therapies, and surgical interventions when necessary, lasting relief and improved ocular health can be achieved.
