Keratoconus Disease: Causes, Symptoms, Diagnosis, and Treatment Options

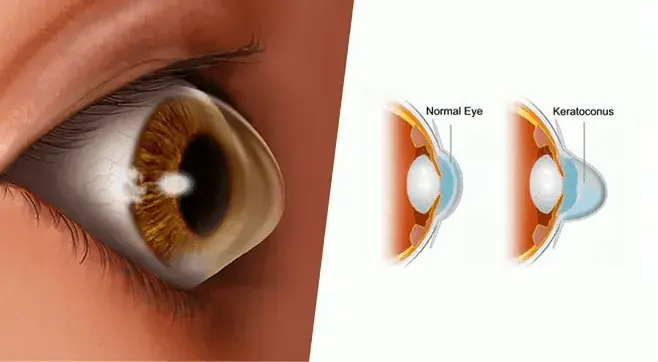
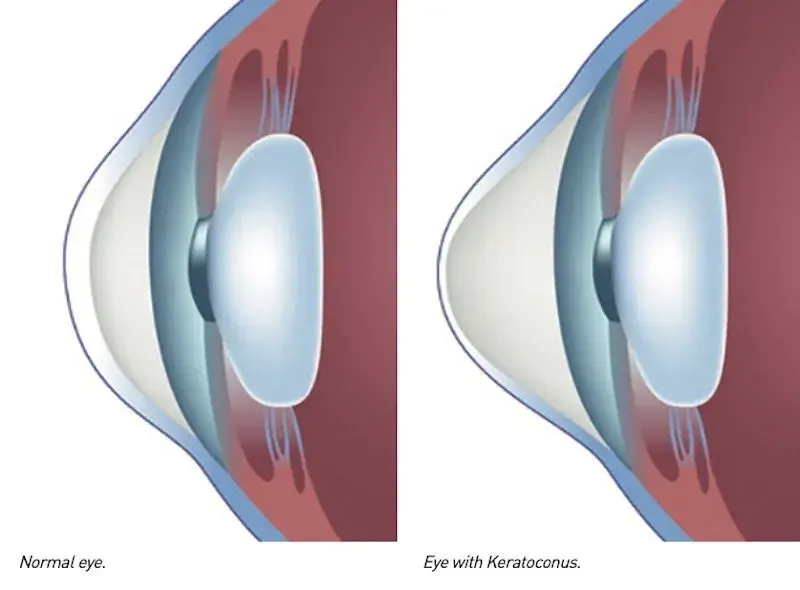
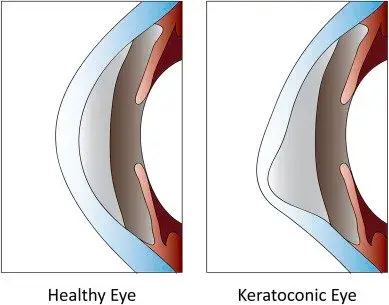
Keratoconus disease is a progressive eye condition in which the normally round cornea becomes thin and gradually bulges outward into a cone-shaped cornea. This change in corneal shape affects how light enters the eye, leading to blurry or distorted vision. In the early stages of keratoconus, vision changes may be mild and correctable with glasses or contact lenses; however, as the disease progresses, vision correction becomes increasingly challenging.
The cornea’s primary role is to focus light onto the retina for clear vision. When the corneal tissue weakens and thins, it loses its regular dome shape. Over time, this irregular shape of the cornea can cause light to scatter, resulting in blurred vision, glare, and difficulty seeing in bright light.
Keratoconus affects people of all ages, but it often begins during the teenage years or early adulthood. Without timely intervention, severe keratoconus can lead to corneal scarring, corneal hydrops, and even the need for a corneal transplant. Understanding this corneal disease is essential for predicting disease progression and protecting future vision.

Common Symptoms of Keratoconus
Patients with keratoconus often experience a range of visual and physical symptoms. These can worsen as the disease progresses from mild to moderate keratoconus or into advanced stages of keratoconus.
-
Blurry or distorted vision that cannot be corrected with a regular glasses prescription.
-
Increased sensitivity to bright light and glare, making night driving difficult.
-
Frequent changes in corrective lenses due to unstable vision.
-
Halos around lights and ghost images, especially in low-light conditions.
-
Eye strain and headaches from prolonged visual tasks.
-
Sudden vision loss in severe cases due to corneal hydrops (fluid buildup in the cornea).
Recognizing early symptoms of keratoconus allows for prompt diagnosis and intervention, helping to improve vision and slow the progression of the condition.

Causes and Risk Factors of Keratoconus
The exact cause of developing keratoconus is still unknown, but research points to a combination of genetic and environmental factors that weaken the corneal collagen structure.
-
Family history of keratoconus or other corneal diseases.
-
Vigorous eye rubbing, often linked to allergies or irritation, accelerates corneal thinning.
-
Genetic disorders such as Down syndrome and connective tissue diseases.
-
Chronic eye inflammation affecting the corneal epithelium.
-
Hormonal changes during puberty or pregnancy that impact corneal thickness.
-
History of poorly fitted contact lenses, especially rigid contact lenses, in the early stages.
Being aware of these risk factors can help prevent or delay keratoconus progression, especially in individuals with a higher genetic predisposition.
Keratoconus Treated
Keratoconus is treated based on its stage and severity. In mild cases, soft contact lenses or glasses may correct vision; however, as the cornea thins and irregular astigmatism develops, patients may require rigid gas-permeable or scleral lenses.
For progressive cases, corneal collagen cross-linking can prevent future vision loss. Severe keratoconus or corneal scarring may require surgery, such as intrastromal corneal ring segments or a donor cornea transplant. Some patients benefit from wearing hard contact lenses post-treatment to achieve clearer vision.
Keratoconus Diagnosed
Eye doctors diagnose keratoconus through vision tests and imaging, such as corneal topography and corneal tomography. These tools detect early changes, such as when the cornea thins or blurry vision appears due to irregular astigmatism.
Patients wearing hard contact lenses may need to remove them to ensure accurate test results. Early detection is vital, as timely treatment can prevent future vision loss and reduce the need for a cornea transplant from a donor.
How Keratoconus is Diagnosed
An eye doctor can detect keratoconus through specialized tests that assess the corneal shape, thickness, and surface irregularities. Corneal topography and corneal tomography are advanced imaging techniques that map the curvature of the cornea, detecting even early stages of keratoconus before vision changes become noticeable.
Other diagnostic tests include measuring corneal thickness to identify corneal thinning and using slit-lamp examination to detect signs of a cone-shaped cornea, corneal scarring, or corneal ectasia. In posterior keratoconus, the thinning occurs on the back surface of the cornea, making advanced imaging essential for accurate diagnosis.
Predicting disease progression is crucial, as early detection enables interventions such as corneal cross-linking, which can strengthen the corneal tissue and prevent the progression of severe keratoconus.
Treatment Options for Keratoconus
Treatment for keratoconus depends on its severity and the extent to which the disease affects daily life. Options range from vision correction with contact lenses to surgical procedures in advanced cases of keratoconus.
-
Glasses or contact lenses in early keratoconus for mild vision correction.
-
Rigid gas permeable lenses, hybrid lenses, or scleral contact lenses to improve vision when glasses are insufficient.
-
Corneal collagen cross-linking to halt disease progression by strengthening corneal tissue.
-
Intrastromal corneal ring segments to reshape the cornea and improve visual acuity.
-
Deep anterior lamellar keratoplasty or full corneal transplantation for diseased cornea in severe cases.
-
Refractive surgery in select keratoconus patients to correct vision, though this is not suitable for everyone.
Wearing contact lenses in keratoconus requires expert fitting to prevent additional corneal damage and maintain long-term eye health.
Surgical Interventions for Advanced Keratoconus
When vision can no longer be corrected with glasses or contact lenses, and corneal cross-linking is not effective, surgical options become necessary. Corneal transplant and corneal transplantation procedures involve replacing the diseased cornea with healthy donor corneal tissue.
A deep anterior lamellar keratoplasty preserves the patient’s healthy inner corneal layers while replacing only the damaged outer layers. This approach reduces the risk of graft rejection compared to a full-thickness cornea transplant. In severe keratoconus with corneal scarring, a full transplant may be the only option.
Modern surgical techniques, combined with advancements in corneal tissue preservation, have significantly improved outcomes for patients with keratoconus. However, potential risks such as graft rejection, infection, and irregular corneal shape post-surgery require careful monitoring.
Preventing and Managing Keratoconus Progression
While keratoconus cannot always be prevented, early detection and appropriate treatment can significantly slow its progression. Avoiding vigorous eye rubbing is one of the simplest and most effective preventive measures against eye strain. Regular eye check-ups, especially for those with a family history of keratoconus, are essential for detecting changes in corneal thickness and shape.
Wearing well-fitted corrective lenses, managing allergies that cause eye irritation, and protecting the eyes from trauma can also reduce the risk of corneal thinning and further vision loss. In cases of progressive keratoconus, treatments such as corneal collagen cross-linking offer a way to stabilize the cornea and preserve visual acuity.
Outlook for Keratoconus Patients
With timely intervention, most patients with keratoconus can maintain functional vision and avoid severe complications. Advances in diagnostic imaging, scleral lenses, hybrid lenses, and surgical techniques have significantly enhanced the ability to effectively treat keratoconus.
Patients diagnosed early have the best chance of preserving vision, especially with treatments that strengthen the cornea and delay the need for a transplant. Those with severe keratoconus who undergo successful corneal transplantation can often return to daily activities, although they may still require corrective lenses.
By working closely with an eye doctor, monitoring vision changes, and avoiding behaviors that damage the cornea, individuals living with keratoconus can achieve long-term eye health and stable vision.
