Herpes Simplex vs Herpes Zoster Virus: Understanding the Key Differences

When it comes to eye infections, many people are surprised to learn that both the herpes simplex virus (HSV) and the herpes zoster virus (VZV) can be responsible. Despite having similar names, these viruses are very different in how they infect the body, how they spread, and the complications they can cause. HSV is the leading cause of corneal infections worldwide, while VZV is most recognized as the cause of chickenpox and shingles.
In this blog, we’ll explore the differences between herpes simplex vs herpes zoster, their symptoms, risk factors, and treatments. By the end, you’ll have a clear understanding of how these viruses behave, why early diagnosis is critical, and how patients can reduce their risks of complications.
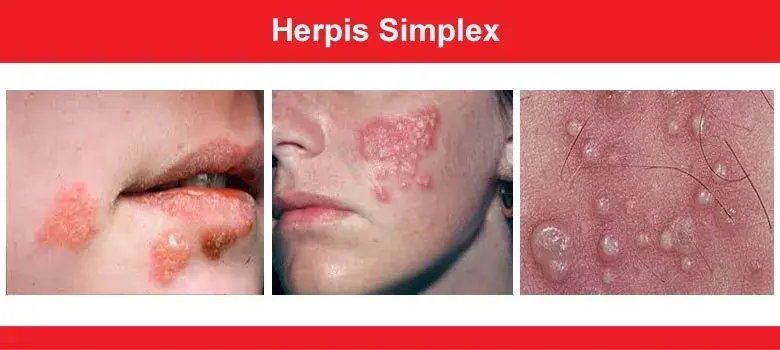
What is Herpes Simplex Virus (HSV)?
The herpes simplex virus is a double-stranded DNA virus that establishes a lifelong infection in the body. There are two main HSV types:
-
HSV-1 (Simplex virus type 1): Most often associated with oral herpes (cold sores, also called herpes labialis) and eye infections.
-
HSV-2 (Simplex virus type 2): Usually causes genital herpes, spread primarily through sexual intercourse and intimate contact.
After the primary infection, the virus hides within neuronal cells of the dorsal root ganglia. From there, the virus can remain silent for long periods but may reactivate due to triggers such as stress, fever, or a weakened immune system. When the virus reactivates, it can cause herpetic lesions, including painful blisters or corneal ulcers.
HSV eye disease is a significant cause of corneal blindness in developed countries. Patients experiencing HSV infection in the eye often report redness, pain, tearing, blurred vision, and a burning sensation.
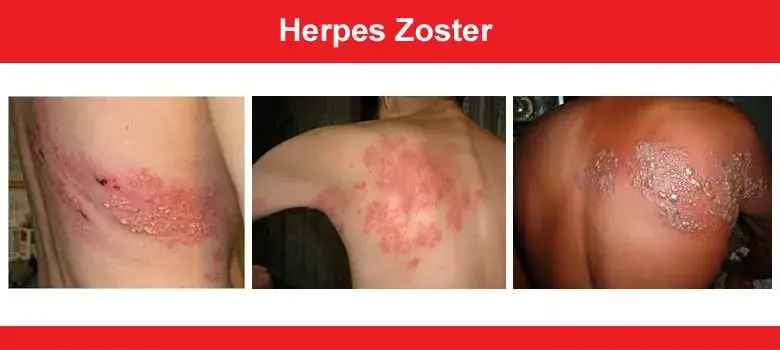
What is Herpes Zoster Virus (VZV)?
The herpes zoster virus, also known as the varicella zoster virus (VZV), is the same virus that causes chickenpox. After a person develops chickenpox, the virus does not fully leave the body. Instead, it enters a state of varicella zoster virus latency in the dorsal root ganglia, much like HSV.
Years later, the virus may reactivate, leading to a shingles outbreak. Shingles occurs when the dormant virus becomes active again, often triggered by age, other health conditions, or a weakened immune system.
A shingles infection typically starts with flu-like symptoms followed by a blistering rash. When shingles occurs near the eyes, it is called herpes zoster ophthalmicus, a serious condition that can threaten vision. The presence of lesions on the tip of the nose (known as Hutchinson’s sign) is highly predictive of eye involvement.
Unlike HSV, shingles is not caused by intimate contact. Instead, it happens when the virus reactivates inside the same person who once had chickenpox.
Key Differences Between HSV and VZV
-
Causative Agents
-
HSV = Herpes simplex virus type 1 or type 2,
-
VZV = Varicella zoster virus (the cause of chickenpox and shingles),
-
-
Mode of Transmission
-
HSV spreads through direct contact, including oral herpes, sexual intercourse, and intimate contact.
-
VZV is acquired first through chickenpox infection, then reappears as shingles when the virus stays dormant and later reactivates.
-
-
Clinical Presentations
-
HSV = cold sores, genital herpes, herpetic eye infections (dendritic ulcers, keratitis).
-
VZV = chickenpox in children, shingles rash in adults, painful fluid-filled blisters, and risk of postherpetic neuralgia.
-
Symptoms of HSV Infection vs Shingles Outbreak
The symptoms of HSV infection and a shingles outbreak differ significantly, although both may involve painful skin and eye lesions.

HSV Infection Symptoms:
Patients with HSV may experience oral herpes (painful blisters around the lips), genital herpes, or eye involvement such as dendritic ulcers. The first outbreak is often the most severe, while recurrences may be milder. Some patients experience flu-like symptoms, swollen glands, and multinucleated giant cells on laboratory testing.
Herpes Zoster Infection Symptoms:
In shingles, patients usually feel flu-like symptoms before the rash appears. The shingles rash develops into shingles blisters, often forming a stripe on one side of the body. The affected skin is painful, and patients describe a burning sensation even before the blisters heal. When the face or eyes are affected, complications can be serious and long-lasting.
Risk Factors for Reactivation
-
Herpes Simplex Virus Reactivation Triggers:
-
Stress, fever, sunlight, or weakened immune system
-
Other health conditions or medications that reduce immunity
-
Pregnant women are at higher risk of severe infection
-
-
Herpes Zoster Virus Reactivation Triggers:
-
Aging and natural decline in cell-mediated immunity
-
Immunosuppressive therapy, chemotherapy, or chronic illnesses
-
Patients who did not receive the chickenpox vaccine or varicella vaccine are more likely to develop shingles
-
Treatment Options for HSV and VZV
Both herpes simplex virus (HSV) and herpes zoster virus (VZV) infections require prompt medical attention to prevent vision loss and long-term complications. The mainstay of management is antiviral medications, most commonly acyclovir, valacyclovir, and famciclovir.
These drugs work by interfering with viral proteins, preventing the virus from multiplying and shortening the duration of active infection.

HSV Treatment
In HSV eye infections, doctors may prescribe either topical eye drops or oral antiviral medications. In some cases, long-term suppressive therapy is recommended to reduce recurrence and reduce transmission to others.
If the infection involves the cornea, careful management with antivirals is critical. The use of steroids must be closely monitored, since inappropriate use in HSV keratitis can worsen scarring or delay healing.
VZV Treatment
When zoster occurs, early antiviral therapy is key. Shingles treatment is most effective if started within 72 hours after the painful rash appears. Medications such as acyclovir reduce the severity of the outbreak, shorten healing time, and lower the risk of complications such as postherpetic neuralgia.
Because shingles often follows the course of the trigeminal nerve when it involves the face, treatment may also require pain relievers, lubricating eye drops, and, in some cases, steroid therapy to control inflammation in the eye. Patients with severe or widespread infection may need hospitalization, particularly if a disseminated infection is suspected.
Prevention: Can You Prevent Shingles or HSV Outbreaks?
Prevention strategies differ depending on whether the virus is HSV or VZV.
Preventing HSV:
The best way to lower risk is by avoiding direct contact with herpetic lesions during outbreaks. This includes abstaining from intimate contact or sexual intercourse when blisters are present.
Patients with oral herpes should not share utensils, drinks, or lip products during an active infection. In patients who suffer from frequent recurrences, doctors may prescribe suppressive antiviral therapy to keep outbreaks under control.
Preventing VZV:
The most effective prevention strategy is vaccination. The chickenpox vaccine (varicella vaccine) protects children against the initial primary infection, while the shingles vaccine is recommended for older adults and those with weakened immune systems.
Studies, including findings from a systematic review, have shown that the shingles vaccine not only helps to prevent shingles but also reduces the risk of long-term nerve pain such as postherpetic neuralgia. Widespread vaccination also decreases the chance of disseminated infection in vulnerable groups, making it a critical tool for public health.
Long-Term Outlook and Patient Support
For patients living with herpes simplex or herpes zoster, the long-term outlook depends on early treatment, preventive care, and overall health. While the virus remains dormant in nerve cells, careful management can greatly reduce complications. With modern antiviral medications such as both acyclovir and valacyclovir, flare-ups are usually well-controlled.
Most patients recover fully from individual outbreaks, though some may need ongoing care if eye damage or nerve pain develops. Importantly, many patients benefit from counseling and education about recognizing triggers, starting treatment early, and protecting others from transmission.
By staying informed and working closely with eye specialists, patients can lead healthy, fulfilling lives while minimizing the risks of future reactivation.
Final Thoughts: Patient-Centered Care for Lifelong Infections
Both the herpes simplex virus and the herpes zoster virus establish lifelong infections in the body. While they share the ability to lie dormant in the dorsal root ganglia and later reactivate, their patterns of transmission, symptoms, and prevention strategies are distinct.
The most important message for patients is that early antiviral treatment can dramatically reduce the severity and complications of both conditions. For patients with HSV, regular follow-up, lifestyle awareness, and sometimes suppressive therapy can help protect vision and quality of life.
For patients at risk of shingles, vaccination remains the most effective way to prevent shingles, lower the chance of a painful rash, and avoid complications like postherpetic neuralgia.
