Corneal Transplant Surgery Brisbane Queensland

Dr Brendan Cronin is a Brisbane-based ophthalmologist and leading eye surgeon and cornea surgeon specializing in cornea transplantation. A corneal transplant, also known as a corneal graft, involves replacing a diseased cornea or damaged or diseased cornea with a healthy donor cornea or healthy donor tissue from someone who has generously donated their eyes through the Queensland Eye Bank.
This incredible act of generosity helps restore vision for patients suffering from cornea scarring, corneal diseases, corneal edema, severe corneal damage, and other conditions that cause vision loss.
The cornea is unique among other organs because it lacks a blood supply. As a result, a transplanted tissue is less likely to be rejected compared to organs like kidneys or lungs. Most patients require only steroid eye drops as part of post operative care to prevent graft rejection.
What Is Cornea Transplant Surgery?
A cornea transplant surgery is a surgical procedure performed when the clear window of the eye, the cornea, becomes cloudy, scarred, or swollen, leading to blurred vision, refractive errors, or significant astigmatism. During the procedure, the surgeon removes the damaged or diseased cornea and replaces it with a new healthy cornea from a donor. The healthy stroma and endothelium intact are carefully sutured into place, allowing light to pass clearly to the retina and helping improve vision.
Donor corneas come from individuals who registered as eye donors before passing away. The donated healthy donor tissue is collected, screened, and stored at the Queensland Eye Bank before being matched with patients in need. This gift of sight is life-changing and is treated with the utmost respect by the surgical and healthcare teams.

Why You Might Need a Corneal Transplant
Not every case of vision problems requires a transplant. Often, laser vision correction, laser eye surgery, or cataract surgery may be enough. However, when these treatments fail, cornea transplantation may be the only way to restore vision. Common reasons include:
- Cornea scarring caused by infection, trauma, or previous surgery
- Eye infection leading to thinning and vision loss
- Fuchs’ dystrophy, a degenerative condition of the endothelial layer or diseased endothelium
- Severe corneal damage after injury or disease
- Complications from previous refractive errors or laser vision correction
- Rare conditions requiring an artificial cornea transplant or stem cells
Patients may also require surgery if they have had retinal detachment, failed corneal grafts, or advanced corneal edema. Without treatment, these conditions can lead to progressive vision loss and reduced best-corrected vision.
Benefits and Risks of Corneal Transplant Surgery
Like any eye operation, corneal transplantation has benefits and risks.
Benefits include:
- Restoring functional vision and clarity
- Helping relieve pain from eye infection or corneal ulcers
- Improving visual acuity and improve vision
- Helping patients return to daily activities and improve their quality of life
Risks include:
- Lifelong chance of graft rejection
- Slow healing process due to a lack of blood vessels
- Risk of infection or complications, such as increased eye pressure
- In rare cases, the need for another transplant if rejection occurs
Your experienced surgeons and healthcare team will carefully assess your eye health to minimise risks and improve outcomes.
Types of Corneal Transplants Available
Dr Cronin performs a wide range of endothelial transplants and corneal grafts, tailoring each procedure to the individual patient’s needs. The main types include:
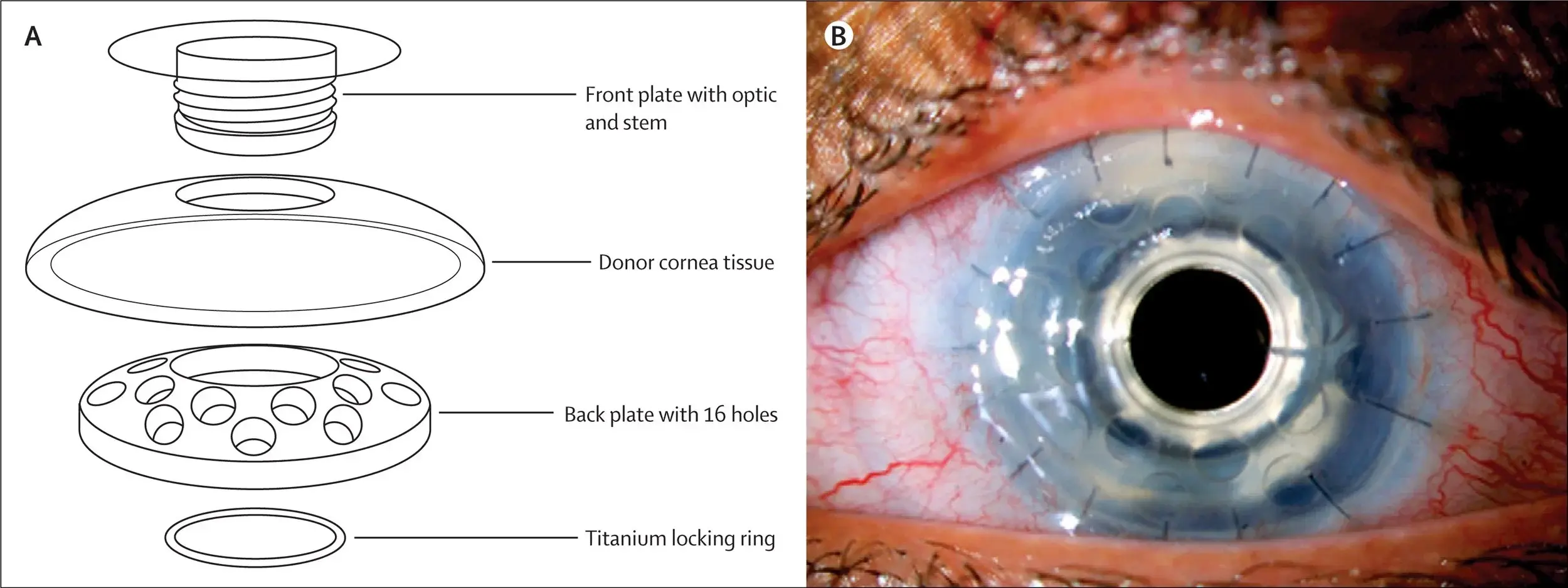
Penetrating Keratoplasty (Full-Thickness Transplant)
This traditional method involves removing the entire thickness of the cornea with a circular blade called a trephine. A donor cornea of similar size is stitched into place, usually with 16 sutures. The stitches are left in place for 18 months or longer to allow the eye to heal. This is often chosen when there is full thickness cornea transplant or extensive corneal damage.
Deep Anterior Lamellar Keratoplasty (DALK – Partial Thickness)
In a partial thickness transplant procedure, only the front and middle layer of the corneal layers are transplanted, while the patient’s own endothelium intact is left in place. This reduces the chance of graft rejection. DALK is useful for patients with cornea scarring but a healthy endothelium.
Descemet’s Membrane Endothelial Keratoplasty (DMEK – Endothelial Transplants)
DMEK is a modern technique, usually performed for Fuchs’ dystrophy or other endothelial cells diseases. Only the innermost layer is transplanted. The graft is floated into position using an air bubble and UV light, allowing for faster healing, minimal stitches, and superior visual recovery compared to older techniques.
Artificial Cornea and Stem Cell Treatments
In rare cases where donor tissue is unsuitable, an artificial cornea transplant may be used. Clinical research is also exploring stem cells and clinical trials as future solutions for complex cases.
The Corneal Transplant Surgery Process
The procedure is typically performed in a hospital under local or general anaesthesia.
- The surgeon removes the outer layers or the entire damaged cornea or diseased tissue, depending on the type of graft.
- The new cornea is stitched or floated into place using an air bubble, or in advanced cases, an automated endothelial keratoplasty technique may be used.
- An eye patch or wear protective eyewear is worn for a few days after surgery.
Most patients can return home the same day, but follow-up with the surgical team is essential.
Recovery Process and Aftercare
Recovery after a corneal transplant can take time, and patience is crucial. Vision may remain blurred initially, but visual recovery continues as the eye heals.
- Stitches often remain in place for over a year.
- Steroid eye drops are used to prevent severe infection and reduce pain.
- Patients should avoid strenuous activity, wear protective eyewear, and maintain a healthy weight to promote optimal healing.
The recovery process is closely monitored by your eye doctor. Regular check-ups ensure the healing process is on track and that the new cornea remains healthy.
Recognising and Managing Cornea Rejection
Even with modern surgical techniques, there is always a risk of cornea rejection due to the body’s immune system. Symptoms can be remembered with the acronym RSVP:
- Redness
- Sensitivity to light
- Vision reduction
- Pain
If you notice these warning signs, see your eye doctor immediately. Quick treatment with steroid drops can often stop rejection and protect your transplanted cornea.
Alternative Treatments and Vision Correction Options
Not every patient requires a corneal transplant. Alternatives may include:
- Contact lenses to manage irregular vision caused by corneal scarring
- Femtosecond laser or other refractive surgery in selected cases
- Partial thickness procedures like DALK, when only certain layers of the cornea are affected
- Artificial cornea for patients unsuitable for donor tissue
Your surgical team will assess your condition and recommend the best treatment plan to restore vision and maintain long-term eye health.
Support and Access to Corneal Transplant Surgery
Accessing a full-thickness corneal transplant or other procedures depends not only on medical need but also on support systems and resources. The National Eye Institute and similar organisations worldwide continue to fund research to improve outcomes for patients needing cornea replacement.
In Brisbane and across Queensland, patients can often use private health insurance to help cover the cornea replacement cost, follow-up appointments, and medication. With advances in surgical techniques and donor availability, more patients are regaining good vision and enjoying restored independence after treatment.
Why Choose Dr Brendan Cronin for Corneal Transplants in Queensland
Dr Brendan Cronin has extensive experience performing all forms of corneal transplant surgery, from full-thickness grafts to advanced endothelial transplants like DMEK or automated endothelial keratoplasty. Patients from across Queensland trust him for his precision, compassion, and commitment to long-term vision outcomes.
Supported by a dedicated healthcare team, Dr Cronin provides expert surgical care, comprehensive aftercare, and ongoing support throughout the recovery process. His goal is not just to improve eyesight but to restore independence, confidence, and quality of life.
